What Are Pressure Ulcers
Pressure Ulcers, also known as decubitus ulcers, are ulcers that develop due to constant pressure on the skin and underlying tissue in the area. Decubitus ulcers usually appear on weight-bearing parts of the body and are common in people who have medical conditions that limit their movement or who are forced to sit or lie in certain positions for long periods of time (bed rest).
The main cause of decubitus ulcers is constant and continuous pressure on the skin and underlying tissues. This pressure cuts off blood flow to the area, which in turn causes tissue death and possible ulceration.
Risk Factors for Pressure Ulcers
Factors that can increase a person's risk of developing pressure sores include:
- Immobilization
- When a person is limited in their movements or unable to move at all, pressure on the skin and tissues can increase.
- Missing position change
- If a person does not change positions often enough when sitting or lying down, pressure can concentrate at a certain point.
- Blood circulation disorders
- Health problems that affect blood flow, such as diabetes, cardiovascular disease, or blocked arteries, can increase the risk of pressure ulcers.
- Unhealthy Lifestyle
- Malnutrition, dehydration, and smoking can interfere with the body's ability to repair tissue and increase the risk of pressure sores.
Classification of Pressure Ulcers
Pressure ulcers are classified according to the severity and depth of the wound. This assessment helps medical professionals plan treatment and understand the extent of damage to the skin and underlying tissue. The following is a classification of pressure ulcers based on the most commonly used system, the National Pressure Ulcer Advisory Panel (NPUAP) Classification System:.
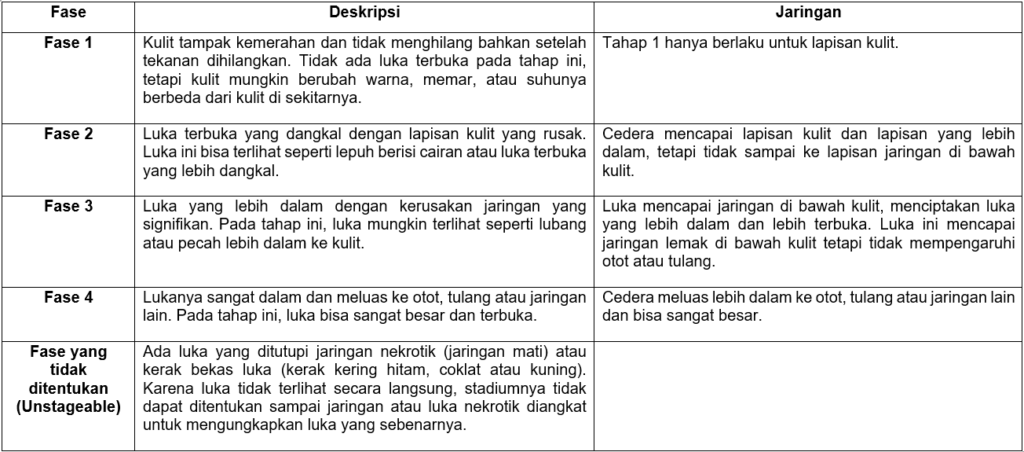
In addition to the above classification system, there are also categories called Deep Tissue Injury (DTI), namely deep tissue injury which can be a precursor to decubitus ulcers. A DTI is an area that feels softer or harder than the surrounding tissue and may be purple or brown in color. DTI is a warning sign of prolonged pressure causing deep tissue damage.
Process of Occurrence of Pressure Ulcers
Decubitus ulcers occur when the skin and underlying tissue are damaged due to prolonged and repeated pressure on an area of the body. The process of developing pressure ulcers includes several consecutive phases. The following are the steps in the decubitus ulcer process:
- Long term pressure
Pressure sores tend to occur in prominent areas of the body, such as the shoulders, spine, hips, heels, and elbows. When a person sits or lies in the same position for a long time without changing their position, long-term pressure can develop in this area.
- Blood circulation disorders
Prolonged pressure on an area of the body causes compression of blood vessels under the skin. As a result, blood circulation is hampered and not enough oxygen and nutrients reach tissue cells.
- Ischemia (lack of blood flow)
Inadequate blood flow causes tissue cells to not receive enough oxygen and nutrients to stay alive and functioning. This leads to a condition called ischemia, where tissue cells begin to die.
- Tissue necrosis (tissue death)
Ischemic conditions that are not treated quickly can lead to necrosis, i.e. tissue death. At this stage, the skin and underlying tissue begin to experience serious damage.
- Inflammation
Tissue necrosis causes the release of inflammatory chemicals that cause inflammation in the area of necrosis. This inflammation can worsen tissue damage and further affect the surrounding tissue.
- Wound Formation
During the process of inflammation and necrosis, the skin and underlying tissue weaken and become damaged. This creates an open wound at the site of inflammation.
- Infection
Open wounds are an entry point for bacteria and other microorganisms. If a wound is not properly cared for and becomes infected, the infection can cause serious complications and slow down the healing process.
- Worsening And Spreading
If not properly treated and cared for, pressure ulcers can get worse and spread to deeper tissue, even muscle or bone. This can cause more serious complications such as bone infections (osteomyelitis) or deformity problems.

Prevention of Pressure Ulcers
Pressure ulcer prevention measures are very important, especially for people who are at high risk of developing the condition. General precautions include:
- When sitting or lying down, change positions regularly to relieve pressure in the same area.
- When sitting or lying down, change positions regularly to relieve pressure in the same area.
- Ensure good nutritional intake and adequate fluid intake to support healthy skin and tissue regeneration.
- Use tools such as pillows and special mattresses designed to reduce pressure on the skin.
The Role of Physiotherapy in Pressure Ulcers Cases
Physiotherapy has an important role in the management and treatment of pressure ulcers. Physiotherapists play a role in helping prevent pressure ulcers in individuals at high risk, as well as assisting in the recovery and treatment of wounds in individuals who have experienced pressure ulcers. Following are some of the main roles of physiotherapy in cases of pressure ulcers:
1. Prevention:
- Risk Evaluation: A physiotherapist can perform a risk assessment to identify people who are at high risk of developing pressure ulcers. By carrying out this assessment, preventative steps can be taken early to avoid injury.
- Edukasi Perubahan Posisi: Fisioterapis dapat memberikan edukasi tentang pentingnya perubahan posisi secara teratur bagi individu yang berisiko tinggi mengembangkan pressure ulcers. Teknik perubahan posisi yang tepat akan membantu mengurangi tekanan pada area yang rentan.
- Pemilihan dan Penggunaan Alat Bantu: Fisioterapis dapat membantu dalam pemilihan dan penggunaan alat bantu, seperti bantal khusus atau alas tidur yang dirancang untuk mengurangi tekanan pada kulit dan jaringan.
2. Treatment and Recovery:
- Evaluation and Treatment Planning: A physiotherapist can evaluate the severity of pressure ulcers and plan an appropriate treatment program to heal the wound. This treatment program may involve a variety of physical therapy approaches.
- Exercise and Movement: Physiotherapists help design safe exercise and movement programs to prevent muscle stiffness and contractures and maintain body strength and flexibility, thereby preventing excessive stress on vulnerable areas.
- Therapeutic Modalities: Physical therapists may use physical modalities such as ultrasound, electrical stimulation, or cold compresses to help reduce inflammation, reduce pain, and speed up the healing process.
3. Education and Counselling:
- Physiotherapists can educate patients and families about the importance of consistent wound care and lifestyle changes to speed healing.
- Assist patients in understanding the importance of self-care, position changes, good nutrition, and pressure management to prevent future recurrence of pressure ulcers.
Also read: Peran Fisioterapi Pada Rheumatoid Arthritis
Reference :
- Guihan M, Hastings J, Garber SL. Therapists’ roles in pressure ulcer management in persons with spinal cord injury. J Spinal Cord Med. 2009;32(5):560-7. doi: 10.1080/10790268.2009.11754561. PMID: 20025152; PMCID: PMC2792462.
- Zaidi SRH, Sharma S. Pressure Ulcer. [Updated 2022 Aug 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553107/
- InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. Pressure ulcers: Overview. [Updated 2018 Nov 15]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK326428/